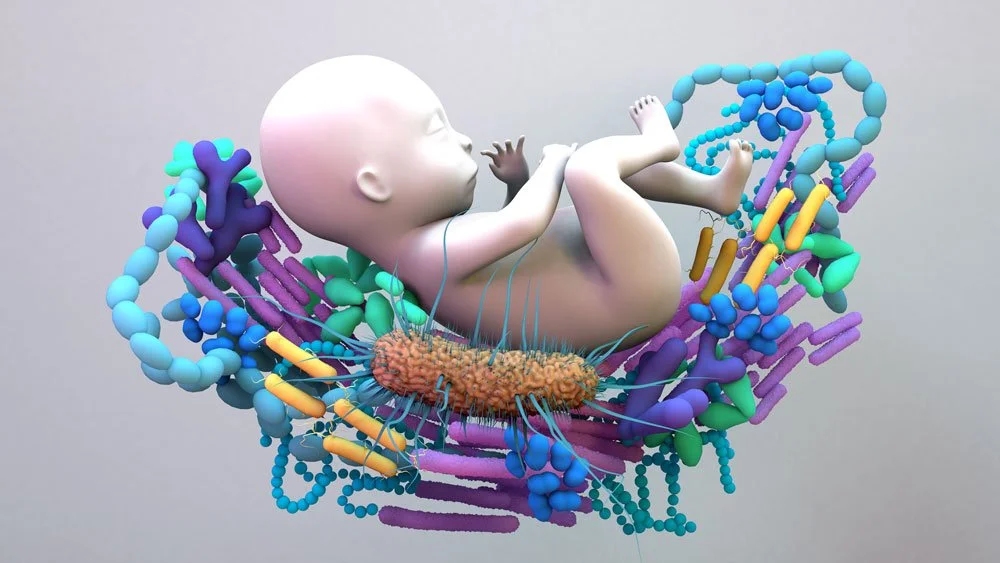
The importance of the maternal/baby microbiome.
In Utero: Prenatal Microbiome Influence
Maternal Microbiome Health
The mother’s gut, vaginal, oral, and even placental microbiomes influence the baby.
A dysbiotic (imbalanced) maternal microbiome can lead to inflammation, impacting fetal development, especially the immune system and brain.
Placental Microbial Exposure
Some studies suggest the placenta harbors microbes (or microbial signals), potentially priming the fetal immune system.
The uterine environment may not be completely sterile, and microbial metabolites from the maternal gut may reach the fetus via the bloodstream.
Immune System Programming
Microbial byproducts like short-chain fatty acids (SCFAs) from maternal gut bacteria can cross the placenta and influence fetal immune development, reducing allergy and autoimmune disease risk.
Epigenetic Influence
Microbial metabolites can also affect gene expression in the fetus, shaping things like metabolism, growth, and neurodevelopment.
At Birth: The Microbial Seeding Moment
Vaginal Birth vs. C-Section
Vaginal birth exposes the baby to the mother’s vaginal and fecal microbiota, kickstarting a robust colonization of beneficial bacteria.
C-section babies are often seeded first by hospital microbes or skin bacteria, and may have a delayed or less diverse microbiome, increasing risk of allergies, asthma, obesity, and type 1 diabetes.
Antibiotics at Birth
Maternal or infant antibiotics disrupt initial colonization.
This may delay or reduce beneficial bacteria like Bifidobacteria.
Delayed Cord Clamping
More than just iron — it may allow more maternal immune factors and even microbes to transfer, aiding immune and microbial development.
After Birth: Feeding & Environment
Breastfeeding
Breast milk contains live bacteria (especially Lactobacillus and Bifidobacterium), prebiotics (HMOs), and immune factors that:
Feed beneficial bacteria
Shape gut flora
Support immune development
Promote gut-brain axis health
Formula Feeding
Often lacks live microbes and has different prebiotic profiles.
Leads to a more adult-like microbiome earlier, with more Clostridium and Enterobacteriaceae species.
Skin-to-Skin Contact
Promotes colonization of healthy skin flora.
Helps reduce hospital-acquired microbes.
Environment
Siblings, pets, dirt, and even rural living introduce microbial diversity that trains the immune system.
Why It All Matters
A well-seeded and nurtured microbiome is linked to:
Lower allergy and asthma rates
Lower risk of autoimmune conditions
Better metabolic health (reduced obesity risk)
Stronger, more balanced immune responses
Better mood regulation and cognitive development (via the gut-brain axis)
* Several probiotic strains have been studied for their ability to reduce the risk of asthma and eczema in babies, particularly when taken by the mother during late pregnancy and while breastfeeding.
Here are the most evidence-backed strains:
Top Probiotic Strains for Preventing Asthma & Eczema in Babies.
Lactobacillus rhamnosus GG (LGG)
Best studied strain for eczema prevention.
Taken in the last trimester and during breastfeeding, it can reduce eczema incidence in high-risk infants.
Supports gut and immune development, modulates inflammation.
Bifidobacterium lactis (B. lactis)
Helps support immune tolerance and reduces inflammatory responses.
Often used in infant formulas as well.
Synergistic with prebiotics (like GOS/FOS).
Lactobacillus reuteri (DSM 17938)
Shown to reduce gut inflammation and promote oral tolerance.
Some evidence for reducing colic and modulating immune responses that may underlie asthma/eczema.
Bifidobacterium longum (especially subspecies infantis)
Colonizes the infant gut very well, especially with breastfeeding.
Promotes anti-inflammatory environment; reduces markers associated with allergic disease.
Lactobacillus paracasei
Modulates Th1/Th2 balance, which is important in allergic conditions.
Used in some combination probiotics to help reduce eczema and upper respiratory tract infections.
What the Research Says
Meta-analyses and Cochrane reviews suggest that taking probiotics during late pregnancy and early breastfeeding can reduce the risk of eczema in infants, especially those with a family history of atopy.
Evidence for asthma prevention is less robust but promising — early immune system education by beneficial bacteria seems key.
Tips for Use in Pregnancy
Ideally, start taking a multi-strain probiotic 3-4 months prior to a conception. The uterine and vaginal microbiomes will be able to enhance a successful conception and implantation. If you have been unaware of the benefits of probiotics and your baby’s health, then supplementing later in the pregnancy, around 32–36 weeks gestation will still bring health benefits. Continue taking probiotics throughout breastfeeding.
Choose a multi-strain probiotic including L. rhamnosus GG, B. lactis, and/or B. longum
Look for products with guaranteed CFU at expiry, not manufacture.
Combine with a healthy diet rich in fiber (which feeds the probiotics) and low in inflammatory foods.